Liver Cirrhosis and Its Impact on Skin: Symptoms Explained
Serving as the body’s powerhouse, the liver is critical for three primary functions: Detoxifying the blood, synthesizing essential proteins, and regulating hormones. When conditions like cirrhosis damage this vital organ, the systemic impact is widespread, often affecting the body’s largest organ: The skin.
For many patients at King’s Transplant Centre, the earliest and most visible indicators of underlying hepatic dysfunction are the dermatological changes they experience. We understand that these outward manifestations—the skin signs of liver damage—can be distressing and confusing.
This comprehensive guide, informed by our extensive experience in advanced hepatology, explains the crucial link between liver cirrhosis and skin health. It helps patients and caregivers recognize the signs of liver damage and understand their management.
The mechanism: Why liver disease affects the skin?
The skin acts as a mirror to internal health. When the liver becomes scarred (cirrhosis), it loses its ability to effectively perform its key metabolic functions.
This leads to a build-up of substances that should have been filtered or metabolized, causing a domino effect throughout the body. The primary factors linking advanced liver disease to skin problems related to liver disease include:
Bilirubin retention (Jaundice): When red blood cells are broken down, they create bilirubin (a yellow pigment) that the liver is incapable of eliminating. Its accumulation in the blood and tissues causes the characteristic yellowing.
Bile salt accumulation (Pruritus): Failed bile flow leads to bile salts depositing in the skin, which irritates nerve endings and causes intense itching.
Hormonal imbalances: A damaged liver cannot properly metabolize hormones, particularly estrogen, leading to vascular and structural changes.
Nutritional deficiencies: Cirrhosis impairs the absorption and storage of fat-soluble vitamins (A, D, E, K) and zinc, critical for skin health, integrity, and wound healing.
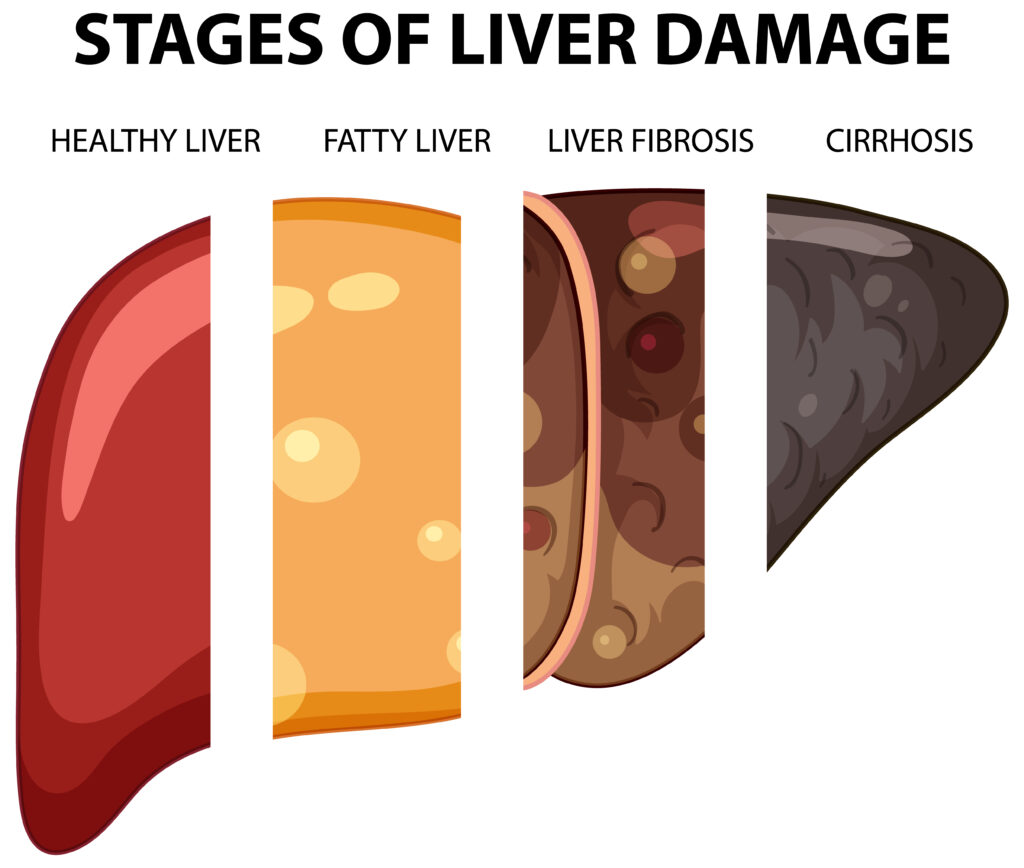
Decoding liver cirrhosis causes
Understanding the underlying pathology is key to recognizing the severity of the skin signs of liver damage.
Liver cirrhosis causes are varied but typically involve chronic, long-term injury to the liver tissue, leading to fibrosis (scarring) and eventual functional failure. The most common causes treated at King’s Transplant Centre include:
- Chronic viral hepatitis: Hepatitis B and C infections.
- Non-alcoholic steatohepatitis (NASH): Often linked to obesity, diabetes, and metabolic syndrome.
- Alcohol-related liver disease (ARLD): Excessive long-term alcohol consumption.
- Autoimmune conditions: Primary Biliary Cholangitis (PBC) and Primary Sclerosing Cholangitis (PSC).
- Genetic disorders: Hemochromatosis (iron overload) and Wilson’s disease (copper overload).
When cirrhosis reaches an advanced stage, the severity of these causes directly correlates with the visibility and persistence of the skin issues with liver disease.
Key signs of liver disease on skin
The signs of liver disease on skin are diverse and can often be the first clue prompting a clinical investigation.
1. Jaundice (Yellowing of skin and eyes)
This is the most classic and recognizable symptom. As the liver fails to process bilirubin, the yellow pigment accumulates in the blood and tissues, causing the skin and the whites of the eyes (sclera) to turn yellow. Persistent jaundice is a powerful indicator of severe, advanced liver damage.
2. Pruritus (Intense itching)
Pruritus is one of the most debilitating skin problems related to liver disease, especially in cholestatic disorders (where bile flow is blocked). This itching is typically generalized, non-rash-like, and often worsens at night.
It is caused by the accumulation of bile salts, which deposit in the skin and stimulate nerve endings. The relentless scratching often leads to skin excoriations and secondary infections.
3. Vascular changes (Spider angiomas and Palmar erythema)
Hormonal and circulatory imbalances caused by liver failure lead to distinct vascular signs:
- Spider angiomas (Spider nevi): These are small, red, web-like clusters of dilated blood vessels with a central spot, often appearing on the face, neck, upper chest, and arms. Their appearance is strongly linked to elevated estrogen levels, which a diseased liver cannot properly metabolize. They are a common skin sign of liver damage in cirrhosis.
- Palmar erythema: This involves noticeable, symmetrical redness on the palms, especially over the padded areas near the base of the thumb and little finger. It is also caused by increased estrogen levels, which lead to capillary dilation.
4. Hyperpigmentation and Xanthomas
- Skin darkening: Patients may notice liver disease and skin darkening, particularly in areas exposed to the sun or where the skin rubs together. This hyperpigmentation results from excessive melanin deposition, influenced by hormonal shifts and sometimes specific conditions like hemochromatosis (which causes a bronze or grayish complexion).
- Xanthomas/Xanthelasma: These are yellowish, fatty deposits that form small bumps, nodules (xanthomas), or patches around the eyelids (xanthelasma). They occur because liver disease can impair the processing of lipids, leading to high cholesterol levels and fat deposits in the skin. They are particularly associated with autoimmune liver diseases like Primary Biliary Cholangitis (PBC).
5. Nail and hair abnormalities
- Terry’s nails: The nails appear mostly opaque or white, with a narrow band of pink or red only at the tip. This is strongly associated with low albumin and is a classic sign of liver damage in advanced cirrhosis.
- Clubbing: The fingertips become enlarged and the nails curve downward, reflecting long-term circulatory and oxygen changes often seen in chronic liver and lung diseases.
- Hair loss: Hormonal imbalances and poor nutritional status contribute to generalized hair thinning and loss of body hair.
How to treat itching from liver disease (Pruritus Management)?
Pruritus can be one of the most debilitating skin issues with liver disease, often resistant to standard treatments. Management focuses on reducing bile salt concentration and blocking the nerve signals that cause the itch:
- Bile acid sequestrants: Medications like Cholestyramine bind to bile salts in the intestine, preventing their reabsorption and promoting their excretion, thereby reducing their accumulation in the skin.
- Rifampicin: This medication is often used because it can activate liver enzymes that help metabolize and clear the itch-causing substances.
- Naltrexone: An opioid antagonist that may help block the central pathways that transmit the itch sensation.
- Topical care: Using cool baths, applying unscented, rich moisturizers, and avoiding extreme heat can provide symptomatic relief. Patients should be encouraged to wear soft clothing and trim fingernails short to prevent skin damage from scratching.
Overview
Advanced management at King's Transplant Centre
It is crucial to understand that while symptomatic treatments can manage the discomfort, they do not cure the underlying cirrhosis. Severe, chronic skin problems related to liver disease often signal that the liver’s functional reserve is critically low.
When symptoms like persistent jaundice and intractable pruritus become severe and medically refractory, it is a clear indicator that the patient may be facing end-stage liver failure.
For patients suffering from advanced cirrhosis and a significantly reduced quality of life, our expert multidisciplinary team at King’s Transplant Centre conducts comprehensive evaluations.
We use advanced diagnostics to precisely assess the degree of damage and determine the optimal time for listing a patient for transplantation. A successful liver transplant replaces the damaged organ, resolving the underlying metabolic dysfunction.
This typically leads to a rapid and profound improvement: Jaundice clears, pruritus disappears, and many other skin signs of liver damage fade, restoring the patient’s ability to sleep and live comfortably.
If you or a loved one is experiencing persistent signs of liver disease on skin, or if previously mild symptoms are worsening, immediate expert evaluation is crucial.
Early diagnosis and timely intervention are key to determining the best course of action—advanced medical management or preparation for transplantation.
Contact King’s Transplant Centre today for a consultation with our specialized hepatology team to assess your condition and discuss the most advanced treatment pathways available.